Category: Transitioning: Other Documents
Results of the sustainability assessment of the HIV response among Key Populations in nine countries of the EECA region in the context of transition from Global Fund support to domestic funding
In 2020, the Eurasian Harm Reduction Association (EHRA), being the part of the Global Fund funded EECA multi-country HIV project “Sustainability of Services for Key Populations in Eastern Europe and Central Asia”, developed a conceptual framework, methodology, and transition monitoring tool to help key populations most affected by HIV strengthen their capacity in monitoring the transition of HIV response from donors’ support (particularly, the Global Fund) to national funding. The assessment is tracking the implementation of government commitments to ensure the sustainable HIV response among key populations within those programmatic areas of a key priority for them.
In 2021, EHRA piloted the developed methodology and tool in nine countries in the EECA region to assess the fulfillment by the governments of their commitments to ensure a sustained response to HIV among key populations in the context of the transition from Global Fund support to national funding. The assessment was conducted in the following countries: Belarus, Georgia, Kazakhstan, Kyrgyzstan, Moldova, North Macedonia, Serbia, Tajikistan, and Montenegro. To implement it, EHRA involved local consultants. National experts from various sectors, including the public sector, communities, and relevant NGOs, were also involved in the assessment in each country.
The 9 reports resulted from the conducted assessments as well as the report providing a brief overview of the results of the assessments are available for download here:
- Assessment report on Belarus (available in Russian only)
- Assessment report on Georgia (available in English only)
- Assessment report on Kazakhstan (available in Russian only)
- Assessment report on Kyrgyzstan (available in Russian only)
- Assessment report on Moldova (available in Russian only)
- Assessment report on North Macedonia (available in English only)
- Assessment report on Serbia (available in English only)
- Assessment report on Tajikistan (available in Russian only)
- Assessment report on Montenegro (available in English only)
- A brief overview of the results of the sustainability assessment of the HIV response among Key Populations in nine countries of the EECA region in the context of transition from Global Fund support to domestic funding (available both in Russian and English)
The results of all 9 assessments were presented to the national partners at the online webinars and also at a number of a different national level thematic meetings. The Global Fund Portfolio Managers working with relevant countries were provided with the assessment reports and informed on the results as well.
In 2022, EHRA is planning to update and improve the assessment methodology and tool based on the results of pilots. And in 2023, the organization will conduct a reassessment in some countries.
Montenegro: Benchmarking sustainability of the HIV response among Key Populations in the context of transition from Global Fund support to domestic funding
The aim of this analysis is to assess the fulfillment of the commitments given by the Government of Montenegro aimed to ensure the sustainability of the HIV response among KPs in the context of the country’s transition from Global Fund support to national funding. The results of the assessment are expected to be used to assist CSO’s, key affected communities and partners to remain more informed and engaged in the monitoring of the transition process from donor to domestic funding and to thereby advocate for the implementation of activities that will lead to the sustainability of the national HIV response.
This assessment was conducted using the Methodological Guide and Transition Monitoring Tool (TMT) developed by EHRA. A number of national commitments contributing to ensuring sustainability of the HIV response were identified and prioritised and subsequently analysed based on available data, as well as information from key informants. The assessment was conducted and led by two national reviewers with the support of local HIV experts and representatives of affected communities from organisations involved in advocacy and service delivery for KAPs and PLHIV (the national reference group).
According to the findings of the study, Montenegro scored as per the following health system domains and programmatic areas shown in Tables below, and colour coded as per the TMT Methodological Guide:
Table 1. Overall evaluation of the prioritized for the assessment commitments by health system domain
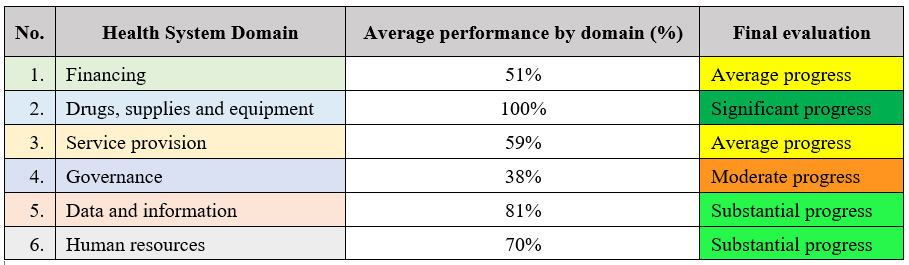
Table 2. Overall evaluation of the prioritized for the assessment commitments by programmatic areas
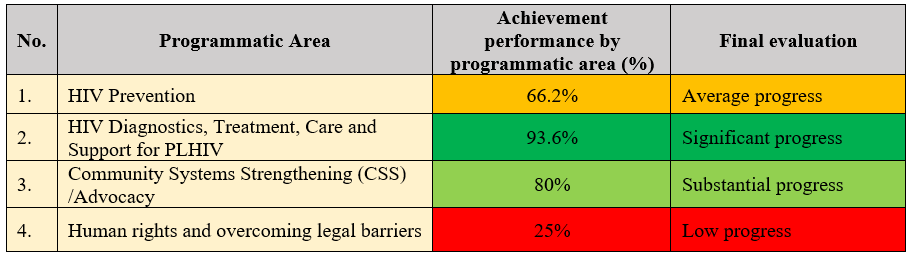
Overall, the scoring in Table 2, above, shows high scores under two programmatic areas but, at the same time, average progress under programmatic area ‘HIV Prevention’ and low progress under programmatic area ‘Human rights and overcoming legal barriers’. In addition, certain challenges under certain health system domains have been identified as shown in Table 1. For example, under the health system domain ‘Governance’, there is moderate progress (38%); under the domain ‘Financing’, average progress (51%); under the domain ‘Service provision’, average progress (59%); while under the domain ‘Human resources’, there is substantial progress (70%). Thus, particular attention and further urgent actions need to be undertaken under the health system domains ‘Governance’, ‘Financing’ and ‘Service provision’, as the lowest performing domains according to the assessment. In addition, further attention and work is required under the health system domain ‘Human resources’. More details on the findings and recommendations can be found under sections ‘Findings’, ‘Discussion and Conclusions’ and ‘Recommendations’ of the report.
North Macedonia: Benchmarking sustainability of the HIV response among Key Populations in the context of transition from Global Fund support to domestic funding
This assessment of the fulfillment of key public commitments with respect to the sustainability of the HIV response among key populations in the context of transition from Global Fund to domestic funding in North Macedonia was conducted using the Methodological Guide and Transition Monitoring Tool (TMT) developed by EHRA. A number of national commitments contributing to ensuring sustainability of the HIV response were identified and prioritised and subsequently analysed based on available data, as well as information from key informants. The assessment was conducted and led by two national reviewers with the support of local HIV experts and representatives of affected communities from organisations involved in advocacy and service delivery for KAPs and PLHIV (the national reference group).
With regards to the fulfillment of the prioritised transition and sustainability-related commitments that were the subject of the analysis, North Macedonia appears to have demonstrated substantial progress in two key domains – financing (progress score of 80%) and service provision (73%); average progress in the domains of data and information (63%) and human resources (55%); moderate progress in governance (43%); and low progress in the domain of drugs, supplies and equipment (0%).
Progress in the fulfillment of the selected transition-related commitments by health system domains in North Macedonia

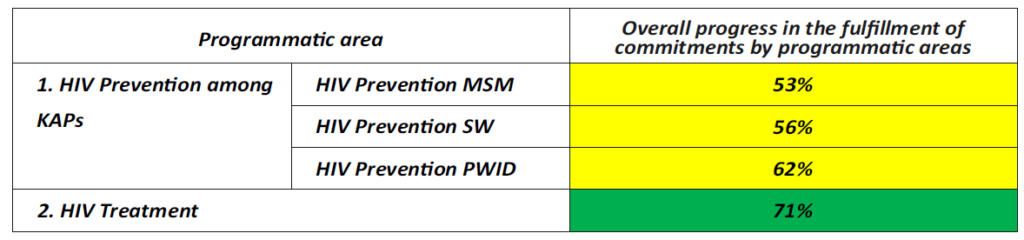
From the point of view of programmatic areas, substantial progress in fulfilling the selected transition and sustainability-related commitments was observed in the area of HIV treatment (progress score of 71%), while average progress was achieved in the area of HIV prevention among KAPs (progress scores of 53% for MSM, 56% for SWs and 62% for PWID).
Progress in the fulfillment of the selected transition-related commitments by programmatic areas
This document should be used to assist CSO’s, key affected communities and partners to remain more informed and engaged in the monitoring of the transition process from donor to domestic funding and to thereby advocate for the implementation of activities that will lead to the sustainability of the national HIV response
Georgia: Benchmarking sustainability of the HIV response among Key Populations in the context of transition from Global Fund support to domestic funding
The assessment of the fulfilment of key public commitments with respect to the sustainability of the HIV response for key populations in the context of transition from Global Fund support in Georgia was conducted based on the Methodological Guide and Transition Monitoring Tool (TMT) developed by EHRA . The assessment aims to assist key affected communities to stay informed and engaged in the monitoring of the transition process and to thereby advocate for the sustainability of national HIV responses.
Findings of Transition Monitoring:
Domain: Results, Impact and Outcome: The transition progress achievement score for three commitments was above 100% which indicates that Georgia has overachieved its goal to control the spread of HIV among the general population and to reduce HIV incidence and AIDS-related mortality. However, progress achieved in terms of containing the HIV epidemic among key populations was impossible to monitor given that no integrated biological-behavioural survey (IBBS) among key populations were conducted during 2019-2020.
Health Domain 1: Financing: The average score for fulfilling commitments under the Financing Domain was set at 67% which implies that average progress was achieved by the government. However, the reliability of the financial data sources used may be questionable. Some indicators measuring the commitments may not capture the real picture in terms of increased financing; while the percentage share of public funding out of total HIV spending has been on the rise, government spending expressed in absolute numbers has declined over the last three years.
Health Domain 2: Drugs, supplies and equipment: The Government has achieved significant progress (with an achievement score of 85%) to ensure the uninterrupted supply of ARVs, OAT medications as well as HIV prevention commodities. However, the ARV prices procured in Georgia remain much higher than reference pricing. Taking into account the budgetary limitations for the healthcare system in Georgia, it can be assumed that overspending on ARVs may limit the fiscal space available for the HIV response. Thus, it seems to be critical to optimise the procurement of ARV drugs to avoid overspending and to make sure that limited resources available for the HIV response in the country are spent most efficiently. In addition, a few episodes of stock-outs of HIV prevention commodities were observed in 2020 that may have been caused by external factors, namely the COVID-19 pandemic and restrictions in transportation and international shipping.
Health Domain 3: Service provision: A high degree of progress in fulfilling the commitments to increase access to HIV services for key populations was documented, with an overall achievement score of 98%. However, this assessment does not provide evidence that no risk to sustainability of services can be expected. The Global Fund support still plays a critical role in expanding or maintaining the scope and scale of HIV essential services provided to key populations, including PLHIV, MSM, PWID, and SW. So far, limited evidence (if any) is available to believe that low-threshold services run by civil society organisations (CSOs), specifically needle and syringe programmes (NSP), community outreach, care and support services, including material support services for key populations, will be sustained beyond the cycle of Global Fund support. There is a declared political commitment from the government about sustainability of all components of the HIV prevention programme, though this declaration has not yet been substantiated with commensurate funding for certain programmatic areas.
Health Domain 4: Governance: A fairly low degree of progress has been achieved by the Government in terms of good governance, with a transition progress achievement score of 27%. The current government, similar to the previous one, has failed to amend punishment-based drug legislation and to create a conducive legal environment. This may jeopardise the sustainability of harm reduction services that currently operate without any legal basis. Adoption, and approval, of HIV prevention service standards for key populations has not been fully realised: only service guidelines had been approved in 2020; approval of service protocols has been delayed; and the costing of HIV prevention services has not yet been developed.
Health Domain 5: Data and information: There is a declared political commitment from the Government about ensuring the sustainability of the second-generation surveillance studies among key affected populations; however, no investments have been made by the Government until now to progressively absorb the cost of IBBS/population size estimate (PSE) studies. Perhaps the Government has been slow to invest in research because there has been constant support from the Global Fund to cover the cost of IBBS and PSE among key population groups.
Health Domain 6: Human resources (HR): No progress (achievement score of 0%) has been achieved. It seems that addressing the challenges related to human resources in health, including in the HIV field, has not been perceived as a priority issue by the government. There were few interventions proposed in the Transition Plan, such as adopting a policy for the continuous professional development of human resources for HIV/AIDS; defining professional competencies and qualification frameworks for various specialists; and accreditation/re-certification procedures, etc. It should be noted that none of these objectives has been realised up to now.

This document should be used to assist CSO’s, key affected communities and partners to remain more informed and engaged in the monitoring of the transition process from donor to domestic funding and to thereby advocate for the implementation of activities that will lead to the sustainability of the national HIV response
The impact of the Global Fund’s Eligibility Policy on access of KAPs to HIV services in Romania
Article:
The impact of the Global Fund’s Eligibility Policy on access of KAPs to HIV services in Romania
Recent revision of the Global Fund’s eligibility policy could give a chance to Romania to become considered as an eligible for HIV allocation within the next allocation period
Doing much for HIV treatment but not for prevention
The HIV story in Romania has been marked by several dramatic episodes. The first was in late 1980s, when thousands of children got infected with HIV through dramatic nosocomial HIV epidemic, predominantly among orphans and hospitalized children.[1] Then the voices of parents and many supporters led to the introduction of the country’s large treatment programs – early on with donor support – to provide HIV treatment to all in need. Today, the country spends 70 million euros for HIV treatment[2], care and support reaching universal access and covering 12,247 people with HIV out of 15,212 as on 2017 which is a great achievement.
But when it comes to prevention – “the Romanian authorities practically invest no money in HIV prevention”, says Nicoleta Dascalu, project manager from the Romanian Association Against AIDS. That is why becoming ineligible for Global Fund’s support of HIV became another dramatic episode in Romanian HIV history.
Consequence of improperly planned transition from donors’ support in Romania
At the beginning of 2010, the country, a fresh member of the European Union, was praised for reaching out to people who inject drugs and even starting a pilot of opioid substitution therapy and needle exchange in prisons. This work was supported by the Global Fund as well as by the Dutch government through UNODC. However, both funding streams stopped in 2010-2011 and the government did not take over funding for NGOs. At the same time, the drug scene also changed with emerge of new psychoactive substances that were legal but could result in up to 10 times injections a day. While the legislative and policy environment in Romania did provide for harm reduction and other services targeted to key populations to be maintained, the Government had shown little commitment to fund such interventions, especially needle and syringe programs. “Most NGOs that had implemented harm reduction services just closed them down, because of lack of funding. The only services that continued were funded, by sheer luck, with money from European Union structural funds projects, dedicated to social and professional reintegration of drug users”, remembers Nicoleta Dascalu.
HIV prevalence among people who inject drugs started growing rapidly: from 3.3% in 2009 to 27.5% in 2013.[3] It was noted in a January 2016 article in the International Journal of Drug Policy that “a specific HIV outbreak among drug users (around 2011) has been directly linked to the significant decline in harm reduction services following the Global Fund transition out of the country[4]“.
Another part of the Romanian HIV story is that HIV prevalence among men who have sex with men also became high. In the EU funded study SIALON II[5], Bucharest recorded the highest HIV prevalence among the 13 cities in study – 18%. Nevertheless, as the country’s official report on the progress of implementation of UN Political commitments on HIV[6] acknowledges, there were no real programs remaining among MSM as on 2016.
Reasons of ineligibility of Romanian HIV component for Global Fund’s support
Since 2007, there has been a requirement in the Global Fund’s Eligibility Policy that in order for UMICs to be eligible for HIV funding, they must have at least high HIV disease burden and also be on the Organisation for Economic Co-operation and Development’s (OECD) Development Assistance Committee (DAC) List of Official Development Assistance (ODA) recipients. The list includes all low, lower middle and upper-middle income countries based on GNI per capita as published by the World Bank, with the exception of those being G8 members, European Union (EU) members, and countries with a firm date for entry into the EU making them ineligible to receive ODA. This requirement is the only reason why Romania lost its eligibility to receive funding for HIV response from the Global Fund and never became eligible again since 2010 when its last Global Fund HIV grant came to an end. At the same time for some reasons this requirement is not applicable for TB and Malaria components thus Romania is eligible to receive the Global Fund funding for TB response and currently is implementing Global Fund’s TB grant. For the 2017-2019 allocation period, Romania was one of only two countries in the entire world (the second one is Bulgaria) being not eligible because of this requirement as they joined the EU in 2007.
Theoretically Romania could become eligible if it met the requirements of so called “NGO rule” – another provision of the Global Fund’s Eligibility Policy which allows for potential eligibility for UMICs that meet the disease burden thresholds for HIV but are not on the OECD DAC List of ODA Recipients. Eligibility under this rule till recently was linked to the existence in country of “political barriers” which preclude the provision of evidence-informed interventions for key populations. Funding provided under this rule must be channeled through civil society and cannot directly fund governments.
In practice the “NGO rule” to date has allowed only one country to be funded – the Russian Federation – in the 2014-2016 allocation period. Romania could have been eligible for the 2014-2016 and 2017-2019 allocation periods, but according to the Global Fund “was not deemed to have substantive political barriers that would preclude providing services to key populations”.
Attempts to influence the situation
Romanian NGOs have tried few times to prove the Global Fund their right to receive an allocation for Romanian HIV component in accordance with “NGO rule”. In 2013 a targeted application for HIV grant was developed and submitted by Romanian NGOs to the Global Fund within the “NGO rule” but was not supported because the Global Fund Secretariat has considered the situation in Romania as a result of ‘lack of funding or political will rather than political barriers’, per se[7].
Another attempt was made in 2016 – a Joint statement of Romanian civil society organizations[8] was sent to the Global Fund’s Executive Director and Fund’s Board in advance to its Thirty Sixth Meeting urging the Board to prevent zero allocation for the HIV component for Romania for the next three years. But their voice has not being heard and Romania was allocated zero funding for the 2017-2019 period.
The last attempt was done in May 2018 when more than 40 international, regional and national organizations addressed[9] the members of the Global Fund Board on the eligibility related issues in advance to its Thirty Ninth Meeting. In their statement, among other issues, civil society organizations called the Global Fund Board not to restrict access to funding for HIV for countries not on the OECD DAC List of ODA specifically appealing to the case of Romania. In the opinion of the subscribers of the statement, “by continuously preserving this requirement the Global Fund itself creates a political barrier that precludes the provision of evidence-informed interventions for key populations in these countries”.
Also, in the same statement the organizations called for the revision of the language of the “NGO Rule” on “political barriers” as this terminology has no clear definition, is inconsistent with international law and could be interpreted against the interests of key affected populations in countries.
Revised Policy – the same eligibility status
One of the result of this Global Fund’s Thirty Ninth Meeting was approval of the Revised Eligibility Policy. In the revised version of the document the OECD DAC ODA Requirement unfortunately was left as it was before but the term “political barriers” in the provision on the exception to the OECD DAC ODA Requirement for HIV/AIDS was replaced with just “barriers” with a note that eligibility for funding under this provision will be assessed by the Secretariat as part of the decision-making process for allocations. It further clarifies that as part of its assessment, the Secretariat will look specifically whether there are laws or policies which influence practices and seriously limit and/or restrict the provision of evidence-informed interventions for key populations.
It is not clear yet if this replacement of the term “political barriers” with just “barriers” will somehow influence the chances of Romania to receive an allocation for its HIV component within the next allocation period but probably not much. As before it will be the Global Fund Secretariat to decide if there are demonstrated barriers in country to providing funding for interventions for key populations, as supported by the country’s epidemiology. And it is clear from the clarification note that as before when considering the eligibility under this provision the Global Fund Secretariat will probably look not if representatives of key affected populations actually have access to the required for them HIV prevention services of a certain quality and at a needed scale but will still consider the existence of the laws and policies which restricts provision of such services by the government.
The only chance to Romanian HIV component to become ever eligible again – is the elimination of the OECD DAC ODA Requirement for HIV/AIDS in the Eligibility Policy. “By keeping the OECD DAC ODA Requirement for HIV/AIDS components the Global Fund continues to restrict access of Romanian NGOs to vitaly needed funding which could allow to ensure an appropriate HIV response among key affected populations“, – says Dragos Rosca, the Executive Director of the Romanian Harm Reduction Network.
At the same time in the opinion of Nicoleta Dascalu from the Romanian Association Against AIDS “it is not the Global Fund responsibility to support AIDS prevention services in Romania, and, if Romania becomes eligible again, the new project should include a strong advocacy component, that should pressure national responsible institutions and make them fund prevention.”
[1] Dente K, Hess J. Pediatric AIDS in Romania – A Country Faces Its Epidemic and Serves as a Model of Success. Medscape General Medicine. 2006;8(2):11.
[2] the HIV treatment/patient/year in Romania is around 6,000 euro (https://ecdc.europa.eu/sites/portal/files/documents/HIV%20treatment%20and%20care.pdf p. 6)
[3] EMCDDA (2016). Statistical Bulletin. Table on HIV Prevalence accessed at: www.emcdda.europa.eu/data/stats2016#displayTable:INF-108
[4] http://www.ijdp.org/article/S0955-3959(15)00236-4/fulltext
[5] EU-funded project Sialon II. Report on a Bio-Behavioural Survey among MSM in 13 European Cities. Accessed at: http://www.sialon.eu/data2/file/133_Sialon%20II_Report%20on%20a%20Bio-behavioural%20Survey%20among%20MSM%20in%2013%20European%20cities.pdf
[6] Romania: Country Progress Report on AIDS Reporting period January 2015 – December 2015. Bucharest, April 2016. Available at: http://www.unaids.org/sites/default/files/country/documents/ROU_narrative_report_2016.pdf
[7] The Impact of Transition from Global Fund support to Governmental Funding on the Sustainability of Harm Reduction Programs. A Case Study from Romania. Eurasian Harm Reduction Network. 2016.
[8] Joint Statement from Romanian civil society urging Global Fund to maintain funding http://rhrn.ro/en/joint-statement-romanian-civil-society-organizations-advance-thirty-sixth-meeting-global-fund-board/
[9] Joint Statement of Civil Society Organizations in advance of the Thirty-Ninth Meeting of the Global Fund Board http://eecaplatform.org/en/joint-statement-of-civil-society-the-global-fund-board/
This text is the author’s version of the article published at www.aidspan.org
The sustainability of the results of the last Global Fund HIV grant for Russia are under a threat
Article:
The sustainability of the results of the last Global Fund HIV grant for Russia are under a threat
Although Russia could become eligible again for the Global Fund HIV funding and even receive allocation within the next allocation period
Conflict of interest: the author of the article is a member of the Coordinating Committee which was responsible for coordination and oversight of the implementation of the Global Fund HIV grant in Russia being discussed in this article.
Background
By the end of implementation of its round-based model of grants’ distribution the Global Fund has invested more than 250 million USD within the Round 3, Round 4 and Round 5 HIV and TB grants to ensure the sustainable response to HIV and TB epidemics in Russia.
A 2010 study by Russian Federal AIDS Center estimated that less than 1% of key populations had access to HIV prevention programs in Russia. The majority of programs providing HIV prevention services to key populations in Russia were dependent on foreign funding. By 2014, the implementation of HIV programs financed by the Global Fund, including those targeted on key populations came to an end. The Russian government didn’t take any steps to fund or even acknowledge the need for HIV programming for key marginalized and criminalized populations, PWUD, SW and MSM/LGBT despite all those promises given by the Minister of Health in 2008 to step in and start paying for such services once the GF programs ended[1].
In light of this situation, the Global Fund has approved the 12 million USD HIV Program in Russia for the period 2015-2017 which was supported within the so called “NGO-Rule” – a provision within the Global Fund’s Eligibility Policy which allows for potential eligibility for UMICs that meet the disease burden thresholds for HIV but are not on the OECD DAC List of ODA Recipients. Local NGO Open Health Institute (OHI) was selected as the Principal Recipient (PR) to continue the activities initiated under two recent HIV programs supported by the Global Fund in Russia and to “create [an] environment for integration of…evidence-based programs into the national HIV strategy”, and to “strengthen the communities of Key Populations in order to increase their involvement in the dialogue with the authorities”[2].
Program details and its uniqueness
This program consisted of three intertwined components: HIV service delivery for PWID, SW and MSM, community systems strengthening (CSS), and removing legal barriers (RLB). From 2015 the activities included services for 17 PWID programs, 5 MSM, and 5 SW. Additionally, in both 2016 and 2017, 12 programs were co-financed and 20 more were given small grants for overcoming legal barriers and rights defense. By the end of its implementation the grant had shown very good results against the targets set (102% average performance of all indicators) and was rated B1, with eight out of ten of its indicators rated A1[3]. A 17 July 2017 Global Fund management letter[4] especially commended “increased mobilization of key affected populations…through the Community Systems Strengthening module,” and praised the Removing Legal Barriers Module for “[showing] excellent results and… contribut[ing] to increasing literacy of key affected populations to help them access health services or navigate through a punitive legal environment”.
The uniqueness of this project is that it was developed and implemented by the forces of the NGOs and communities’ representatives only, without any involvement and support from the governmental sector. The Coordinating Committee (analogue to CCM but without involvement of the governmental sector) was established by the civil society based National Dialogue to coordinate the implementation of the project. “The Coordinating Committee brought together key populations groups, groups of people living with HIV, NGO representatives and human rights advocates who had previously not found common ground, enabling them to forge a common platform and agenda”, says Victoria Dollen, Secretary of the Coordinating Committee.
Also, within the implementation of this project each key population group created sustainable key populations monitoring mechanisms (key populations Forums) to ensure key populations engagement into the meaningful dialogue with the government at all levels.
Reminding about the HIV situation in Russia and its impact on the EECA Region
The region of Eastern Europe and Central Asia (EECA) is the only region in the world where the HIV epidemic continues to grow[5], and Russia could be considered as a „driving force” of the epidemic in the region. According to UNAIDS 2018 Global AIDS Update “the HIV epidemic in Eastern Europe and central Asia has grown by 30% since 2010, reflecting insufficient political commitment and domestic investment in national AIDS responses across much of the region. Regional trends depend a great deal on progress in the Russian Federation, which is home to 70% of people living with HIV in the region. Outside of the Russian Federation, the rate of new HIV infections is stable. Insufficient access to sterile injecting equipment and the unavailability of opioid substitution therapy are stymying efforts in the Russian Federation to prevent HIV infections among people who inject drugs”.[6]
For several years now, there has been a concentrated HIV epidemic in Russia among such key groups affected by HIV as injecting drug users, men who have sex with men and sex workers[7], and in some regions of the country a generalized epidemic among the general population is even being observed[8]. About 70% of all HIV cases in Russia are associated with the use of injecting drugs and still the main way of HIV transmission is parenteral. Recent IBBS research conducted in seven cities of Russia within the implementation of the “NGO rule” HIV Program demonstrates 48,1 – 75,2% HIV prevalence among people who inject drugs (PWID), 7,1 – 22,8% among men who have sex with men (MSM), and 2,3-15.0% among sex workers (SW).[9] With more then 1 220 000 cases being registered as on the end of 2017, the coverage by HIV treatment of PLH in country is about 35%[10].
Given these facts, as well as taking into consideration the geopolitical position of the Russian Federation, the migration flows in the region, etc., it is clear that when planning a response to HIV epidemic in EECA region it is impossible to neglect an HIV situation in Russia and not to support HIV response in this country, as such approach can ultimately reduce to zero all efforts by donors and governments to counteract the HIV epidemic in neighboring countries.
Russia’s eligibility and perspective for sustainability of HIV services
The implementation of this last Global Fund’s HIV grant in Russia has ended on December 31st 2017 with a closure period to end on September 30th 2018. During the Thirty-Ninth Meeting of the Global Fund Board which took place in May 2018 a decision was made to preserve the OECD DAC ODA Requirement for HIV/AIDS in the Global Fund’s Eligibility Policy as well as the exception to OECD-DAC ODA Requirement for funding civil society for HIV/AIDS (formerly referred to as the “NGO Rule”). This means that there is a chance that Russia, as the only country in the world yet which has proved itself eligible for Global Fund’s HIV funding within the “NGO rule”, could be considered eligible under this provision again and may receive an allocation within the next allocation period 2020 – 2022.
Unfortunately, Russia was not eligible to receive any transition funding from the Global Fund to sustain the achievements of this HIV project and now there is a risk that most of the services on HIV prevention that are being carried out by the NGOs within this program, as well as initiatives aimed at advocacy and protection of the rights of representatives of communities, may cease their work in the nearest future, because the funding allocated by the state is not enough to support them, or such funding is not allocated at all.
In addition to inability to receive the transition funding country has lost about 650 000 USD[11] due to the internal regulations of the Global Fund Secretariat according to which all currency translation difference could not be spent on the program activities but should be returned to the Global Fund. This money also could be used to allow the continuation of the key project activities till the beginning of the new allocation period. At the same time the Coordinating Committee has a funding from the Global Fund to till 31.01.2020.
Urgent actions to ensure the sustainability of the project results are needed
The Russian Coordinating Committee is making now the attempts to attract the attention of the Global Fund’s Secretariat and Delegations to the Global Fund to this situation with threat to the sustainability of the results of the recent HIV project by calling to ensure the continuation of HIV prevention services and community-based response in Russia at least until the new allocations for 2020 – 2022 to be announced by the Global Fund Secretariat. There is no any sense to abandon after every three years everything which was achieved with the support of the Global Fund’s funding and then start everything from scratch – this is just a waste of money, time, efforts and lives of people affected by HIV.
“This NGO-Rule Program demonstrated that key affected populations can and in fact should design, implement, and control WHO recommended HIV prevention services among key populations. The Program is a success story and a best practice in creating key populations mechanisms for monitoring of service quality and human rights violations, and to engage key affected populations into the meaningful dialogue with the government”, says Mikhail Golichenko, Senior Policy Analyst from the Canadian HIV\AIDS Legal Network. “This Program was inexpensive tool to contribute to communities’ systems strengthening, support them to overcome the legal barriers and retain KAPs as equal parties in the dialogue with the Russian Government, and as such should not be lost due to the lack of funding”.
[1] S. Shonning. Community Systems Strengthening and Removing the Legal Barriers Modules of the Global Fund Program: Improving access to prevention, treatment and care for key population groups in Russia: Baseline and progress to date Report. January 2017 (on file with the author).
[2] The Global Fund, Charitable Donation Agreement, RUS-H-OHI (on file with the author)
[3] The Global Fund, RUS-H-OHI-RP: 3-SI-762018. Performance Letter Progress Report covering the period 1 January, 2017-31 December, 2017 (on file with the author).
[4] On file with the author
[5] http://www.unaids.org/sites/default/files/media_asset/Global_AIDS_update_2017_en.pdf
[6] UNAIDS 2018 Global AIDS Update. 2018. Online: http://www.unaids.org/sites/default/files/media_asset/miles-to-go_en.pdf
[7] https://www.avert.org/professionals/hiv-around-world/eastern-europe-central-asia/russia
[8] http://www.rbc.ru/society/02/11/2016/581997289a794704fcfaaa79
[9] Federal AIDS Center or Rospotrebnadzor. Information Note. HIV in Russia in 2017. Online: http://aids-centr.perm.ru/images/4/hiv_in_russia/hiv_in_rf_31.12.2017.pdf
[10] Ibid
[11] Presentation by E. Kryanina, ED of OHI (PR of the GF HIV grant) at the meeting of the Coordinating Committee on 07.06.2018. (on file with the author).
This text is the author’s version of the article published at www.aidspan.org
Global Fund grant to Ukraine finds treatment success for multidrug-resistant TB with two-pronged approach
According to the WHO, Ukraine remains a country with a high TB burden, and in 2014 it became one of the five countries with the highest burdens of multidrug-resistant tuberculosis (MDR TB) in the world. The TB epidemic in Ukraine is marked by the spread of multidrug-resistant and extensively drug-resistant tuberculosis (XDR TB), relatively high MDR TB mortality and one of the lowest TB treatment success rates in the region of Eastern Europe and Central Asia – 72% in new TB cases and 38,6% in patients with MDR TB (WHO, 2016).
Currently the Global Fund to Fight AIDS, Tuberculosis and Malaria (the Global Fund) is supporting the implementation of programs to fight tuberculosis in Ukraine within a new country HIV/TB grant for 2018-2020, as well as through catalytic funding. The current program, which started this year, is being based on the previous three-year project, “Investing for Impact against Tuberculosis and HIV”, which had been implemented in Ukraine in 2015-2017 and was completed, with success, at the end of last year.
One of the three key implementers of this project was the Alliance for Public Health (the Alliance), which was responsible for a number of program components, in particular for providing medical and social support to ensure adherence to MDR-TB treatment. Implementation of this latter component achieved high success rates (up to 80%).
Key success factors and outcomes
One of the key factors contributing to the success of this project component was the use of the DOTS approach (Directly Observed Treatment Short-course) in combination with social support for patients, which included the delivery of psychosocial services and training in treatment adherence. This project was implemented in all regions of the Ukraine and performed strongly in all of them.
Apart from the Alliance, other partners involved in implementation included the Public Health Center of the Ministry of Health of Ukraine and the Ukrainian Red Cross Society. The Red Cross Society, which has a wide network of branches covering all the regions of Ukraine, and also has the required number of visiting nurses, was responsible for the DOTS and social support components of the project.
Before patients were released from hospitals, they were asked if they would like to be involved in the project at the outpatient stage of treatment. If the person agreed, information about the patient was given to a relevant branch of the Red Cross Society, where a supervisor was assigned to receive that patient’s TB drugs, attending to the patient daily. If the patient did not miss any doses, he would receive food parcels twice a month.
The efforts of the Alliance and its partners to provide medical and social support to patients and establish their adherence to MDR TB treatment within this project continued the work that had been started in 2013 with the implementation of the previous Global Fund TB grant from Round 9. In 2013, just over 100 patients were enrolled in the support program. Treatment success rates were very high, at 86%, while the treatment success rate for patients with similar conditions who also received treatment within the Global Fund project but were not covered with DOTS or by social support from the Red Cross, was 44% (according to the Alliance).
According to one staff member from the Alliance, one of the reasons for such high treatment success rates was the approach the program used to select patients: at first patients for whom good treatment outcomes were expected were enrolled in the program – ‘treatment-naïve’ patients, patients with repeated TB cases (if the previous TB case was cured) and patients whose first treatment courses had failed. Further, starting from 2014, all patients eligible for the treatment regimens procured within the Global Fund project were enrolled in treatment. After 2015, the patients who received treatment within the state budget were also enrolled in the program.
In 2014, the treatment success rate for the 500 patients covered by the project was 79%, and in 2015 it was 75%. The target for patient coverage in the three years from 2015 to 2017 was 9,300 patients, and was overachieved – the actual number of patients with MDR TB covered by the program was 9,420. (Treatment success rates for the patients enrolled in 2016 will be available later in 2018.
According to Eugenia Geliukh, the program’s project manager, the program can be credited with improving the overall MDR-TB treatment success rates in the country: In 2012 it was 34%, in 2013 it was 39%, and in 2014, 46% (WHO Tuberculosis country profile).
Ensuring sustainability of the TB response in Ukraine
“In three years, we fully piloted the DOTS model combined with social support of the patients and proved the efficiency of this project in Ukraine,” says Andrey Klepikov, Executive Director of the Alliance for Public Health. “Our main message to the government is to make sure that, considering the existing evidence base and taking into account the ongoing processes of transition of TB programs from Global Fund support to domestic funding, this component will also be taken over by the state.” Klepikov suggested that treatment success rates would be halved if, after the withdrawal of Global Fund support, the government supported only drug procurement, without the social support component.
This aspect is crucial as in recent years there has been a rapid transition of the TB response to domestic funding. Until 2017, procurement of half of the second-line drugs to treat multidrug-resistant forms of TB in the country was covered by the Global Fund; starting in 2018, the government took over the procurement of all TB and MDR-TB drugs. Moreover, it is planned that by the end of 2018, 90% of XDR-TB treatment will be covered by domestic funds. The remaining 10% will be procured by the Alliance within Global Fund programming (133 schemes with delamanid).
So far, the equipment for rapid TB diagnostics, supplies and reagents are mainly procured with financial support from the Global Fund and other donors. According to the new Global Fund grant agreement, to implement the 2018-2020 HIV/TB project, every year the procurement of equipment will incrementally be covered from the state budget. Currently, a National TB Program concept has been approved in Ukraine, and it is expected that this year the Parliament will approve the National TB Program for 2018–2021.
Within the new grant, in 2018, support for patients who receive treatment will remain the responsibility of Alliance, in eight regions of the country, with no Red Cross Society involvement. However, it is planned that the social component will also gradually be taken over by the government. In 2018, it is projected that social support for 20% of patients receiving support from NGOs will shift to the Ministry of Ukraine’s Public Health Center. Financial support for this activity will still come from the Global Fund, and the Alliance provides technical support to the PHC within this component. Starting from 2019, 50% of patients will receive support from within the state budget and in 2020, it is expected that 80% of the patients will receive support from the state.
TB treatment approach based on results-based financing model
The Alliance also has implemented a pilot MDR-TB treatment project using a results-based financing (RBF) model. In 2017, the Alliance applied this approach when implementing opioid substitution treatment programs in the Odessa region, within the same Global Fund grant, and decided to adapt it to TB treatment based on the DOTS model. The main goal of the project was to reduce treatment costs per patient per year, and to hand over the implementation of DOTS and social support for TB patients to the primary-care level of the state healthcare system.
“Involvement of the Red Cross Society or other NGOs in DOTS implementation is an interim solution,” says Eugenia Geliukh. “Such projects can be implemented only as long as donors support them. As soon as donors stop financing those activities, NGOs will not be able to continue them at their own expense. At the same time, delivery of treatment services through primary healthcare centres (PHCCs) is in line with the concept of the healthcare reform which is currently going on in Ukraine.”
Within the project, Alliance signed contracts with 14 PHCCs in the Odessa region to implement DOTS and provide social support to patients receiving treatment. The specific mode of providing DOTS services was defined by each PHCC.
Within the pilot project using the RBF model the cost of treating one MDR TB patient for one year was UAH 9,000 (compared to UAH 13,000 for the Alliance project) with the same outcomes. Treatment success rates for the MDR TB patients are not yet available as they have not yet completed their treatment. But for the patients with drug-susceptible TB, the average treatment success rate was 93%, compared to the 35–40% registered in some Odessa region districts before the pilot project implementation started.
This project was not included in the new program supported by the Global Fund for 2018–2020. Moreover, within the new programme the government made a decision to go back to DOTS provision by NGOs and not by state-run primary healthcare institutions. But the city of Odessa became interested in the pilot project’s results. The annual budget of UAH 2,2 million (which is equivalent to $85,000) is allocated within the Odessa city HIV/TB program for 2019–2020, to cover up to 700 people with DOTS through primary healthcare centres. In 2019 half of these funds are expected to be covered by the city budget, and in 2020, 100%.
“In the end, the results-based financing model has been accepted and supported with municipal funding,” said Andrey Klepikov, executive director of the Alliance for Public Health. “It is a great victory for ensuring sustainability and transition. And civil society will remain one of the key players in our national TB response, becoming more and more recognized by the Ukrainian government.”
Source of the original content: http://www.aidspan.org/gfo_article/global-fund-grant-ukraine-finds-treatment-success-multidrug-resistant-tb-two-pronged